What do the following have in common? Patients misrepresenting a non-covered procedure as medically necessary to get insurance to reimburse the cost; unbundling, or billing separately for component pieces of a single procedure; doctors billing the insurance company for a procedure that was never done; providers who are offered incentives to write prescriptions for certain types of drugs; providers who bill for more expensive services or procedures than were performed.
The answer. All are examples of health insurance fraud, waste and abuse (FWA).
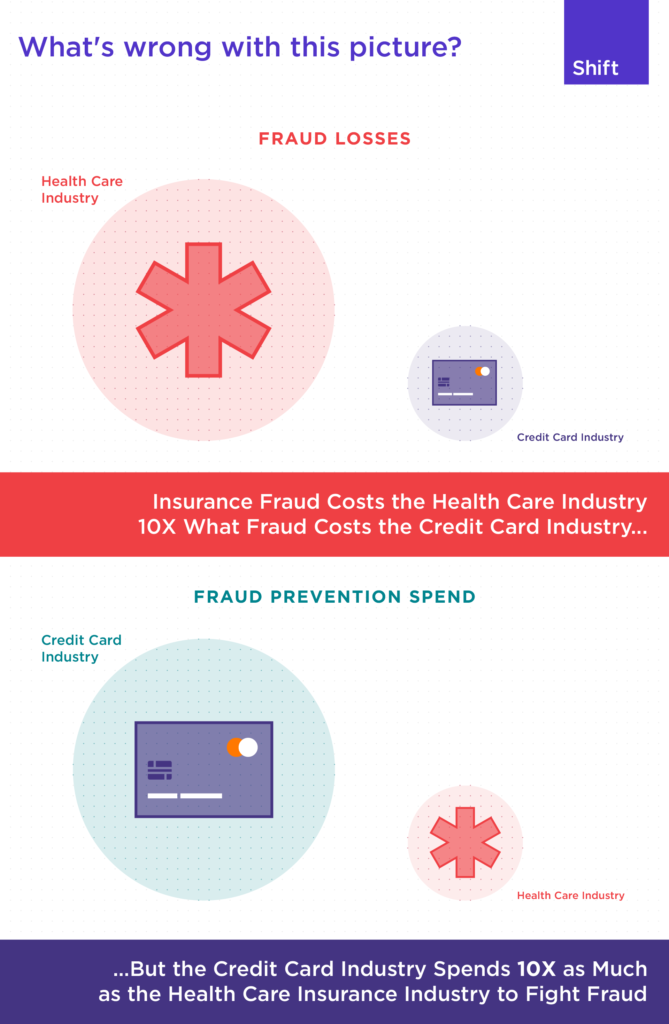
Unfortunately, what this illustrates is that health insurance fraud comes in many shapes and sizes - and costs the industry (and ultimately its policyholders) millions. For example, the healthcare industry loses 100 times MORE to fraud, waste and abuse than the credit card industry loses to fraudulent activities. And yet, the health insurance industry spends ONLY 10% as much as the banking industry does on fighting credit card fraud. In light of this disparity, many health insurance companies are participating in International Fraud Awareness Week to help raise awareness for their, and the industry's, anti-fraud programs.
And fortunately, there is good news on the horizon. An influx of innovative start-ups within the insurance marketplace are actively developing technology designed to assist insurers and administrators in progressing their counter fraud programs. Taking advantage of new data sources, artificial intelligence and SaaS delivery models helps accelerate claim payments, reduce fraud and drive better patient outcomes. Because one dollar wasted or paid out through a fraudulent claim is money that cannot be spent on improving the quality of healthcare.
Using its AI-native technology, Shift is enabling health insurers to reduce fraud losses and improper payments. Money that can now be used to improve healthcare a win-win-win scenario for the patient, provider and health insurance company.


